Applications Open for $50 Billion Rural Health Transformation Program
On September 15, CMS revealed details on applications for the much-anticipated Rural Health Transformation Program (“RHTP”), which was passed as part of the One Big Beautiful Bill (“OBBB”) in July of this year. The RHTP provides $10 billion in annual funding (ending in 2030) to all 50 States to further various objectives directed at strengthening rural hospitals. Not all States will receive the same amount, however, as how a State aligns itself with the goals of the current administration will play a significant role in the amounts it receives.
RHTP Overview
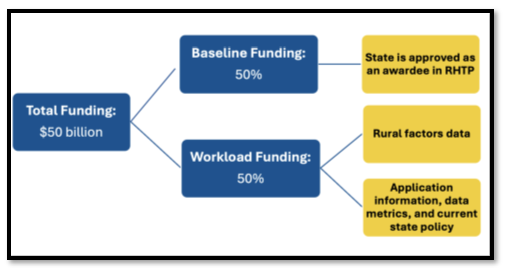
Every State in the country is eligible to receive funding, with half of the $50 billion to be allocated equally among the 50 states (called the “Baseline Funding”) and the remaining half to be allocated based on factors that demonstrate heightened need for the funding – factors which will be demonstrated in the application process (called the “Workload Funding”):
The RHTP can be seen as an answer (or even offset) to the OBBB’s cuts to Medicaid funding, which was anticipated to disproportionately impact rural hospitals. The Notice of Funding Opportunity (“NOFO”) was posted to grants.gov, a website used to apply for federal aid on the same day CMS made its announcement. The RHTP has five stated “goals,” which are slightly expounded upon in the application materials in the NOFO:
- Make rural America healthy again: Support rural health innovations and new access points to promote preventative health and address root causes of diseases. Projects will use evidence-based, outcomes-driven interventions to improve disease prevention, chronic disease management, behavioral health, and prenatal care.
- Sustainable access: Help rural providers become long-term access points for care by improving efficiency and sustainability. With RHT Program support, rural facilities work together—or with high-quality regional systems—to share or coordinate operations, technology, primary and specialty care, and emergency services.
- Workforce development: Attract and retain a high-skilled health care workforce by strengthening recruitment and retention of healthcare providers in rural communities. Help rural providers practice at the top of their license and develop a broader set of providers to serve a rural community’s needs, such as community health workers, pharmacists, and individuals trained to help patients navigate the healthcare system.
- Innovative care: Spark the growth of innovative care models to improve health outcomes, coordinate care, and promote flexible care arrangements. Develop and implement payment mechanisms incentivizing providers or Accountable Care Organizations (“ACOs”) to reduce health care costs, improve quality of care, and shift care to lower cost settings.
- Tech innovation: Foster use of innovative technologies that promote efficient care delivery, data security, and access to digital health tools by rural facilities, providers, and patients. Projects support access to remote care, improve data sharing, strengthen cybersecurity, and invest in emerging technologies.
As a condition for receiving the funds, States must spend them on at least three of the following nine healthcare-focused areas: (1) prevention of chronic disease; (2) provider payments; (3) consumer tech solutions; (4) training and technical assistance; (5) workforce; (6) IT advances; (7) appropriate care availability; (8) behavioral health; or (9) innovative care models (such as developing value-based care). Although States will have wide latitude in how they spend the funding they ultimately receive, the amount of that funding will be determined by how they plan to spend it (and how they follow through with their plan).
Application Details
Given that the Baseline Funding is allocated evenly regardless of application or State-specific factors, States applying for funding will be focused on the “Workload Funding” and the factors that go into it. These factors themselves have both an objective and subjective component, with the objective component being the “Rural Factors Data” and the subjective component being the “Application Information”:
- Rural Factors Data: This includes metrics such as the size of a State’s rural population, the proportion of rural health facilities in the State, the amount of uncompensated care, population in rural areas, geographic distribution of the state (i.e., distance patients must travel for care in rural areas), and the percentage of hospitals that receive Medicaid DSH payments.
- Application Information: This includes factors such as how the State plans to use the funds (so called “programmatic initiatives”), and current State policy. CMS will look at how and whether the State plans to implement integrated care models, promote nutritional goals, restrict SNAP benefits on non-nutritious foods, collaborate with larger health systems, implement licensure compacts, etc.
For the Application Information, CMS will assign a weighted score of 0-100. The States are then re-scored annually and essentially given a CMS report card on subjects like access to health, quality of care, financial trends, workforce data, technology improvements, and program implementation. States can receive more funding for following through with their goals, but they may receive less funding if they do not.
The deadline for States to apply is November 5, 2025, and this is the only opportunity for a State to do so. To apply, each State must submit its own application (and cannot do so jointly with other states), which must come from a State department or agency endorsed by the corresponding governor. CMS will announce the respective State allocations by December 31, 2025.
Reporter, K. Tyler Dysart, Atlanta, +1 404 572 3532, tdysart@kslaw.com.
GAO Releases Report on Urban Hospital Closures and Their Effect on Communities
On September 19, 2025, the Government Accountability Office (GAO) released a report on urban hospital closures and the effects on the community after such closures. Titled “Urban Hospitals: Factors Contributing to Selected Hospital Closures and Related Changes in Available Health Care Services,” the report examines hospitals that closed in 2022 or 2023 (the hospitals are not identified by name) and analyzed HHS data concerning those closures. GAO also interviewed representatives from these five hospitals, along with other stakeholders including representatives from nearby hospitals, other healthcare providers, community organizations, state hospital associations, and local government officials.
GAO found that financial decline in the form of financial losses or declining profits was a factor at all five of the hospitals it studied. For instance, one of the hospitals had been losing millions of dollars each year, and the hospital’s health system owner decided to redirect the funds that it had been using to support the struggling hospital. Another hospital had been the subject of three bankruptcy filings in the five years prior to its closure. All five of the studied hospitals had profit margins that were lower than the median for urban hospitals in the year prior to their closure, and four had margins that were lower than the 25th percentile.
Four of the selected hospitals experienced low or declining inpatient volumes, which can contribute to financial decline, with occupancy rates between 19 and 27%, far lower than the median rate of 64% for all urban hospitals nationally, which results in the hospitals incurring staffing costs without the necessary patient revenue. Hospital representatives cited reduced services, few employed physicians, and competition from a nearby hospital for this low and declining volume. Representatives from some of the hospitals also cited a recent reduction in services, challenges maintaining staffing levels, fewer physician referrals, and a recently opened hospital about five miles away.
All five of the studied hospitals also had aging physical infrastructure that was outdated and costly to maintain, which also contributed to the closures. For instance, one hospital’s campus was over 100 years old, had frequent water leaks due to holes in the roofs and aging pipes, and was in disrepair due to a lack of investment. A hospital representative at one of the selected hospitals estimated that it would cost approximately $50 million in infrastructure spending to make the hospital viable, while CMS Medicare Cost Report data showed that that hospital had lost over $43 million in fiscal year 2021.
GAO also found that ownership and management practices contributed to the closures. For instance, GAO found that two of the five hospitals were not part of a larger health system, which meant less leverage when negotiating payment rates and higher costs for things like electronic health record systems and other investments. Two of the hospitals also had separate owners for the hospital business and the real estate, which may have contributed to closure by impeding the sale of one and imposing financial risks on the other. Inconsistent billing and poorly maintained financial records also contributed to lower revenue at two hospitals.
After closure of the five studied hospitals, availability of inpatient and some outpatient services either shifted or decreased in the hospitals’ communities. Two of the closed hospitals continued to provide some outpatient services or transferred some services to nearby hospitals. Although patients at all five hospitals had alternative providers available, stakeholders interviewed by GAO noted that patients of one of the selected hospitals likely had to travel farther to access certain services, including obstetrics.
The full Report can be found here.
Reporter, David Tassa, Los Angeles, + 213 443 4335, dtassa@kslaw.com.
Upcoming Events
King & Spalding 12th Annual Cybersecurity & Privacy Summit
- Tuesday, September 30 at 10:00 A.M. – 6:00 P.M. ET
In-Person & Virtual
Join King & Spalding for the 12th Annual Cybersecurity & Privacy Summit, an immersive program dedicated to sharing key lessons, best practices, and the latest critical trends shaping the world of cybersecurity and privacy. This year, our theme “Navigating the Future: Empowering Innovation, Protecting Data and Prioritizing Privacy” sets the stage for insightful dialogue and practical guidance.
The Summit will feature distinguished data, privacy and security lawyers; in-house counsel; and leading industry experts who will focus on balancing innovation with risk management, sharing insights into new and upcoming privacy regulations, exploring the evolving threat landscape and more. Mark your calendar and join us for a dynamic program designed to address the most pressing issues in the field.
Further program announcements will follow, with the full agenda to be released in the coming weeks.
For questions or information about registering, contact the K&S Events Team.
King & Spalding Webinar: Managing Managed Care: Updated Dispute Resolution Strategies From Contracting Through Trial
- Wednesday, October 1 at 1:30 P.M. ET
Virtual
Relationships between healthcare providers and managed care organizations (MCOs) are continuously evolving, from trends related to forum selection and claim consolidation in dispute resolution clauses to addressing MCO practices and policies such as chargemaster audits, the Two-Midnight Rule, implants, use of third-party reviewers, ED down-coding, 340B reimbursement and more. King & Spalding’s experienced panel will discuss the significant issues that providers are facing, along with strategies to address them proactively through contracting.
For questions or information about registering, contact Sydney Forte.
King & Spalding Health Law & Policy Forum West
- Wednesday, October 15, 8:30 A.M. – 6:00 P.M. PT
The Ritz-Carlton, Marina del Rey
Join our distinguished faculty and industry leaders for our annual Health Law & Policy Forum West in Marina del Rey. As the healthcare industry continues to evolve in response to economic pressures, patient needs and accelerating technological advances, this full-day program will cover the trending topics that lawyers, executives, managers and investors need to know as they adapt to changes associated with the new administration and more. A keynote session featuring Chad Golder, general counsel of the American Hospital Association, and Rob Hur, former special counsel and U.S. attorney, and current King & Spalding partner, will discuss key issues facing the healthcare industry. Additionally, our partner Rob DeConti, former chief counsel to the Department of Health and Human Services (HHS OIG), will provide his insights into the OIG’s enforcement priorities and share his thoughts on the emerging enforcement trends and compliance issues.
Attendees will also enjoy multiple networking opportunities, including a reception following the sessions. Register by September 29. Registration is available at $95 per person. For questions and to register, contact the K&S Events Team.
Editors: Chris Kenny and Ahsin Azim
Issue Editors: Jenna Anderson